
The future depends on quick and accurate detection of antibodies to determine if subjects have had an immune response to contagious diseases, such as COVID-19 (novel coronavirus).
Two common serological diagnostic methods for novel coronavirus are an enzyme-linked immunosorbent assay (ELISA) and an indirect fluorescent antibody test (IFA).
The direct ELISA method requires a patient’s blood to be drawn and then typically sent to a lab where it is processed into a serum.4 A well plate is then prepared with an immobilized synthetic spike protein with a similar shape to novel coronavirus. The serum is then added to the well plate and the IgM and IgG antibodies bind with the antigen. Unbound antibodies are washed away. A chemical liquid is also added which changes color if antibodies have bound to the target antigen. The color changes at a rate proportional to the amount of antigen-specific antibody in the specimen. Color intensity can be assessed visually or spectrophotometrically with an immunoassay reader (pictured at the top of Figure 2).

The second, and more advantageous serological diagnostic method, is the indirect fluorescent antibody test (IFA).
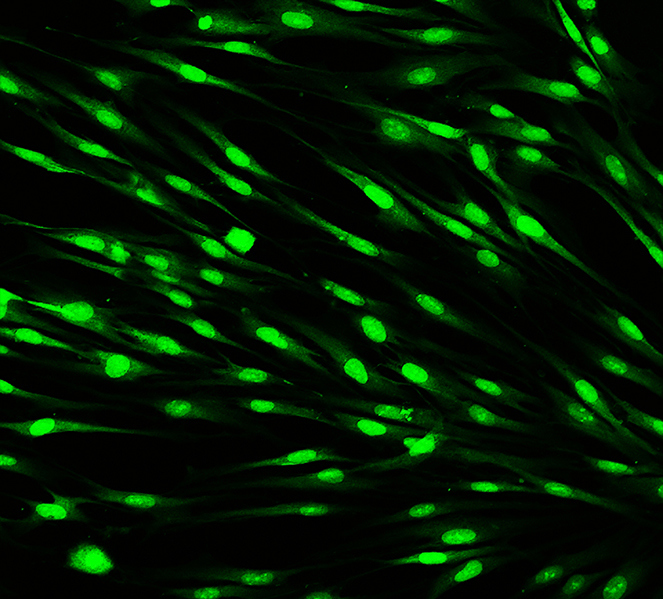
The steps of the IFA are very similar to those of the ELISA. Both virus-infected and uninfected cells are fixed to wells in a glass slide. As with the ELISA method, unbound antibodies are removed by washing. The binding of primary antibodies to the slide wells in the IFA method is demonstrated by using a fluorescent dye-conjugated anti-immunoglobulin. After washing away any unbound conjugate, slides are covered with buffered glycerol and examined with a fluorescence microscope. The morphology and location of fluorescence can be evaluated to differentiate specific reactions from nonspecific reactions (Figure 3). This is not true for most other serological tests and is a major advantage of the IFA method.5
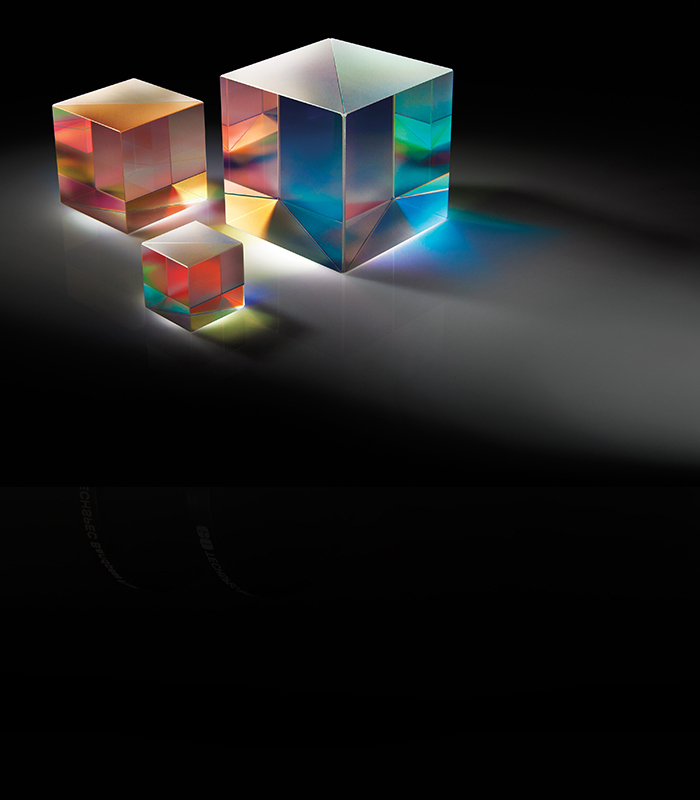
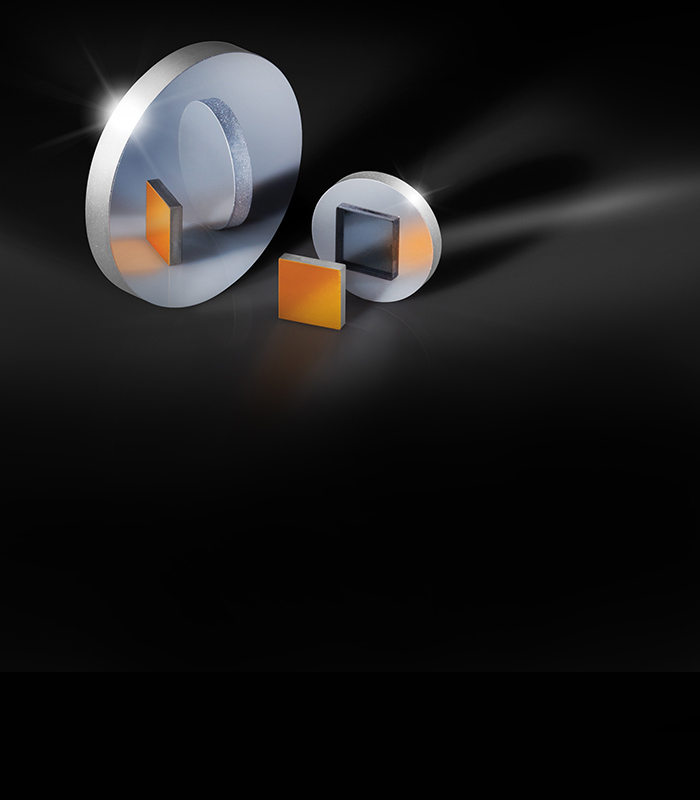
Many immunoassay readers for the ELISA and IFA methods rely on fluorescence or color changes from enzyme reactions and follow a similar schematic to fluorescence microscopes (Figure 4). Examples of prominent companies that support immunofluorescence applications include BioTek Instruments, Molecular Devices, Essen BioScience, and Thermo Fisher Scientific.

An excitation filter allows the passage of wavelengths from an illumination source that would excite the fluorescent sample. These excitation wavelengths reflect off of a dichroic filter and are focused onto the sample by lenses. Fluorescent emission from the sample transmits through the dichroic filter towards lenses that focus the light onto the system’s detectors. Measuring the amount of fluorescence lets the immunoassay reader determine the presence of COVID-19 antibodies that would indicate if a patient had the virus.








or view regional numbers
QUOTE TOOL
enter stock numbers to begin
Copyright 2023 | Edmund Optics, Ltd Unit 1, Opus Avenue, Nether Poppleton, York, YO26 6BL, UK
California Consumer Privacy Acts (CCPA): Do Not Sell or Share My Personal Information
California Transparency in Supply Chains Act